Table of Contents
ToggleHypothyroidism and PCOS – Unlocking the Connection
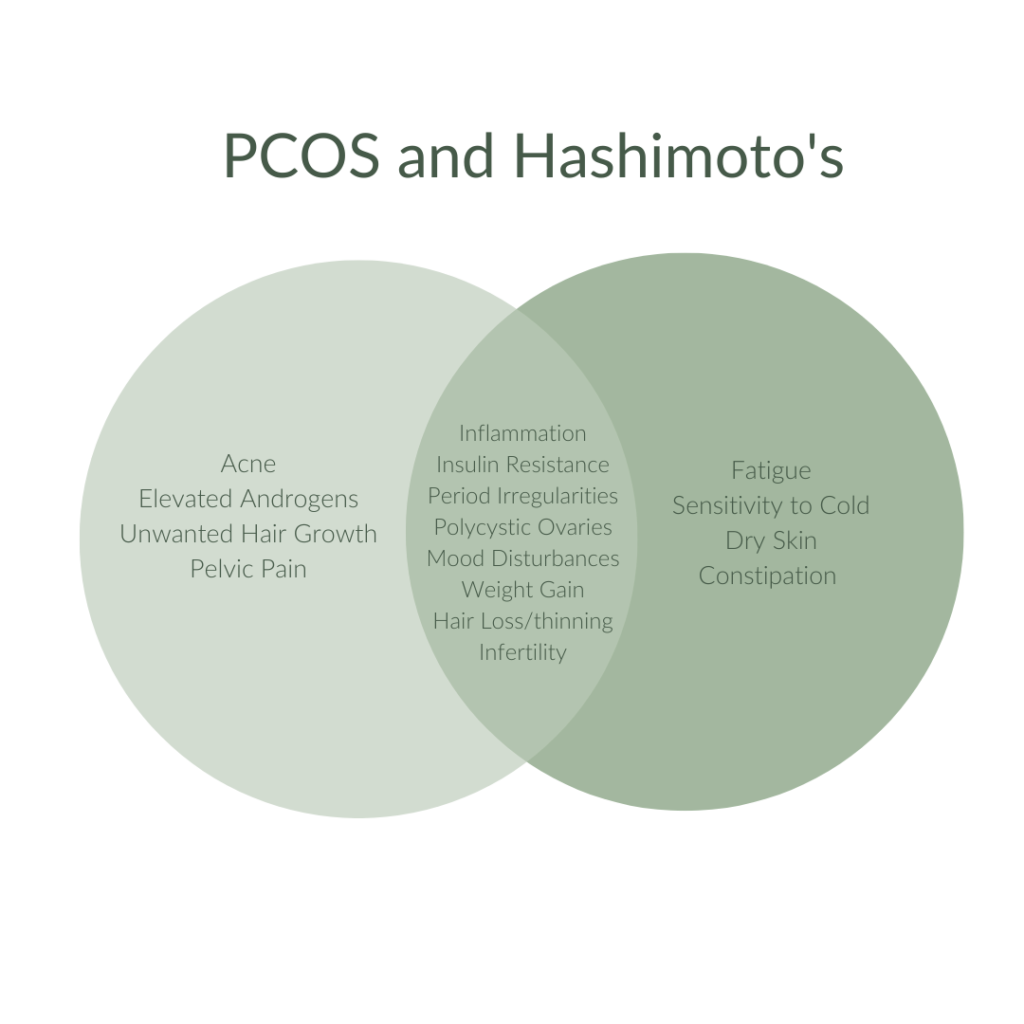
Ever wondered about the mysterious dance between your hormones? Let’s dive into the intriguing world of Polycystic Ovary Syndrome (PCOS) and Hypothyroidism. These two common hormonal rollercoasters have more in common than you might think! While researchers aren’t quite sure how these two conditions are related, it is clear that there is a bidirectional relationship. For example, women with PCOS are three times more likely to also suffer from Hashimoto’s thyroid disease than the general population . At the same time, polycystic appearing ovaries can be a clinical sign of hypothyroidism. Imagine a game of “Who Wore It Best?” but with commonly associated symptoms—it’s like they’re sharing the same closet!
Understanding PCOS
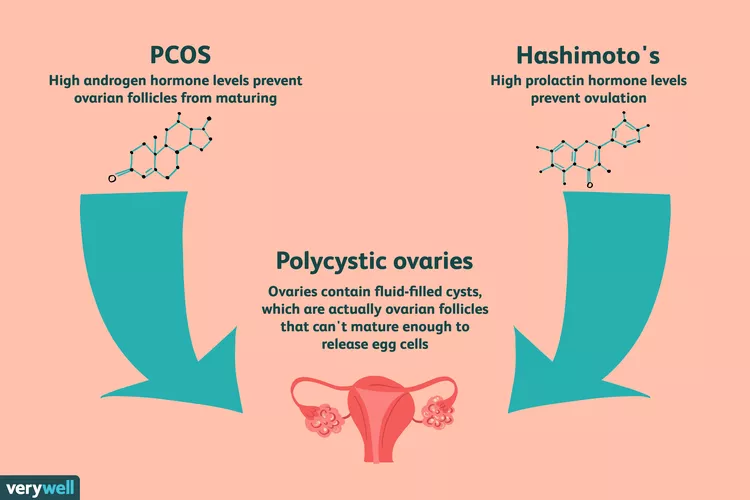
Polycystic Ovary Syndrome (PCOS) is a hormonal imbalance that occurs when your ovaries create excess androgens, causing reproductive hormones to become imbalanced. PCOS causes irregular menstrual periods, excess hair growth, acne, and infertility. In PCOS, many small fluid sacs develop along the ovary’s outer edge. These small fluid-filled cysts contain immature eggs called follicles that fail to regularly release eggs.
PCOS is not known to have an exact cause. The primary causes are insulin resistance, excess androgens, obesity, and inflammation. It is also more likely for women to develop PCOS if their mother or sister has PCOS or type 2 diabetes .
Understanding Hypothyroidism
Your thyroid is a small, butterfly-shaped gland in the front of your neck that secretes two important hormones—thyroxine (T4) and triiodothyronine (T3)—which control the way the body uses energy. Hypothyroidism, or underactive thyroid, is a condition in which your thyroid gland doesn’t make enough thyroid hormones to meet your body’s needs.
Factors that cause hypothyroidism include Hashimoto’s (an autoimmune disease and the most common cause), thyroid gland inflammation, congenital hypothyroidism, radiation therapy, insufficient iodine in your diet, certain medications, and surgical removal of the thyroid gland.
The Link Between Hypothyroidism and PCOS
To fully understand the link between thyroid disorders and PCOS, it is crucial to answer two essential questions:
-
What Happens to Ovaries in Thyroid Disorders? Hypothyroidism affects the ovaries similarly to PCOS, causing the enlargement of the ovaries and the formation of cysts due to a rise in TSH levels which leads to increased collagen deposition within the ovaries .
-
What Happens to the Thyroid in PCOS? Patients with PCOS often present with elevated levels of thyroid autoantibodies. Studies have shown a higher presence of autoimmune thyroiditis (AIT) in patients with polycystic ovary syndrome .
Importance of Accurate Diagnosis
It is essential to exclude the possibility of hypothyroidism before making a definitive diagnosis of PCOS. Hypothyroidism can be difficult to diagnose and may be missed in women with PCOS unless a complete diagnostic evaluation is performed. On its own, a high TSH level is not diagnostic of hypothyroidism. Therefore, T3, T4, and thyroid antibodies tests, along with TSH, should be screened for an accurate diagnosis to find optimal treatment options and avoid further complications. This is especially important in young women because both disorders are connected with fertility problems.
Ovarian Health,
Hypothyroidism and PCOS
Both PCOS and hypothyroidism can cause anovulation—regular periods without the release of an egg from your ovaries. LH (Luteinizing Hormone) and FSH (Follicle Stimulating Hormone) are the two hormones that regulate how your ovaries function. In PCOS, the LH/FSH ratio is higher compared to those without PCOS, and similarly, LH/FSH is higher in Hashimoto’s thyroiditis.
In PCOS, abnormal levels of the pituitary hormone (LH) and insulin resistance are major factors responsible for increased levels of male hormones (androgens), which interfere with the normal function of the ovaries, causing infertility. Further, excess androgens get converted to testosterone in the adipose tissue and are aromatized to estrogen in fat tissue .
Insulin Resistance and Weight Gain in Hypothyroidism and PCOS
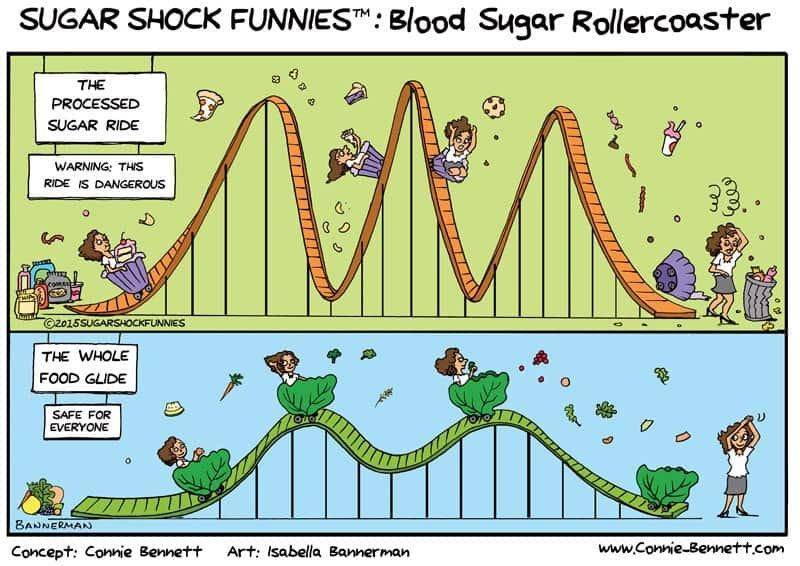
Insulin helps control the amount of glucose in the blood. With insulin resistance, body cells do not respond normally to insulin, leading to glucose buildup in the blood. An increase in BMI along with an increase in abdominal obesity generally correlates with insulin resistance and PCOS, seen in a large majority (54-68%) of PCOS cases .
Not all people with high BMI are insulin resistant; this association is mainly represented by the presence of visceral/central adipose tissue. Many studies show that blood levels of TSH are higher in people with increased visceral adipose, leading to rapid reproduction of fat cells, weight gain, inflammation, leptin resistance, and further insulin resistance .
TIP: Exercise is a terrific insulin sensitizer as it helps muscles use blood sugar for movement. HIIT training can work wonders here!
Managing Hypothyroidism and PCOS
Here are a few ways to start healing and balancing your hormones:
Improve Your Gut Health
Gut health plays a huge role in hormonal health by balancing your sex hormones like estrogen and reducing inflammation. If you constantly face gut issues, your body will not absorb the nutrients required for the proper functioning of the thyroid gland. Healing the gut is essential for treating the root cause of Hashimoto’s and PCOS.
- Include a variety of colorful fruits and vegetables.
- Understand and remove food sensitivities (e.g., gluten, dairy, soy, corn, processed foods, and fatty foods).
- Remove gut irritants like caffeine and alcohol.
- Include prebiotic-rich foods like curd, pickled vegetables, sauerkraut, kimchi, and kombucha.
- Ensure adequate hydration.
- Spend time in nature and engage in physical activity.
Balance Your Blood Sugar Levels
Balancing blood sugar levels should be a top priority for overcoming PCOS and autoimmune Hashimoto’s thyroiditis. Eating balanced meals with adequate amounts of lean protein, healthy fats, and complex carbohydrates helps stabilize blood sugar levels, vital for hormonal harmony, energy, and weight.
- Avoid sugary candies, colas, ultra-processed packaged food items, and bakery items.
- Stay hydrated; drinking water reduces glucose concentration, helping to stabilize blood sugar levels.
- Regular exercise helps reduce high blood sugar, improve insulin sensitivity, and stabilize blood sugar levels.
Add Anti-Inflammatory Foods
Anti-inflammatory foods can significantly impact managing PCOS and hypothyroidism:
- Fresh fruits, vegetables, and green leafy vegetables should be staples in your diet.
- Use herbs and spices like ginger, garlic, cloves, turmeric, oregano, cardamom, black pepper, fenugreek seeds, and cinnamon.
- Introduce good quality fats like nuts, seeds, and avocados into your diet.
- Include Omega-3-rich foods like salmon, trout, tuna, flaxseeds, chia seeds, and walnuts.
- Switch from commercially refined vegetable oils to good quality filtered or cold-pressed oils like groundnut, mustard, sesame, coconut, olive oil, and ghee.
TIP: To reduce excessive salt and sugar, use herbs and spices to improve texture, provide deep flavors, and enhance the taste of any dish!
Balance Your Lifestyle
Although it may seem overwhelming to adopt a new lifestyle, taking it one step at a time can lead to sustainable and healthy transformation. Lifestyle has a tremendous effect on your health, especially with PCOS and Hashimoto’s.
- Get enough sleep to reduce hunger, stress, and inflammation.
- Engage in regular physical activity to maintain good health.
- Find healthy ways to reduce stress, such as meditation, yoga, and breathing exercises.
- Listen to your body and be kind to yourself.

Seek Help for Hypothyroidism and PCOS
If you are dealing with Hypothyroidism and PCOS, don’t go solo; these conditions may require medical intervention from your healthcare practitioner. Following a personalized nutrition plan from a certified nutritionist can be beneficial.
Conclusion
Studies conclude that hypothyroidism and PCOS frequently occur together, with thyroid disorders, especially Hashimoto’s thyroiditis, being more common in women with PCOS than in those without. The exact nature of this link is not yet fully understood. Imagine PCOS and hypothyroidism as partners in crime in a thrilling mystery novel, causing hormonal havoc and sharing symptoms like secret agents. Don’t let their antics steal the show. Be the hero of your hormonal tale and take charge of your health by making positive lifestyle changes, nurturing your gut, and practicing good nutrition to prevent long-term complications.
Remember, this blog is your treasure map, not a diagnosis. Always consult your healthcare professional before making any health-related decisions. Now go forth and conquer, hormone hero!
For more insights on managing PCOS and hypothyroidism, visit Nourish Fit.
References:



